Dr. Josh Redd DC, MS, DABFM, DAAIM
The ‘Long Haulers’ Protocol
Dr. Josh Redd DC, MS, DABFM, DAAIM
The ‘Long Haulers’ Protocol
What to do AFTER you’ve been infected with Covid-19
(and tips to lower your risk of catching it or to become more resilient if you do get it)
If you came in with Covid symptoms I would use many of the same approaches I use with my autoimmune patients, which is to restore and balance immune health through addressing the whole health of the body.[1]
The most important place to start is validating your experience. Most people feel like they are going crazy when they start to have strange and chronic symptoms. Their doctors, family, and loved ones often reinforce this by brushing off their symptoms because they don’t understand them or know what to do. My goal is to educate you about what’s going on with your body to remove the fear that so often accompanies mysterious symptoms. This will help you feel more empowered to address your health.
What to do AFTER you’ve been infected with Covid-19
(and tips to lower your risk of catching it or to become more resilient if you do get it)
If you came in with Covid symptoms I would use many of the same approaches I use with my autoimmune patients, which is to restore and balance immune health through addressing the whole health of the body.[1]
The most important place to start is validating your experience. Most people feel like they are going crazy when they start to have strange and chronic symptoms. Their doctors, family, and loved ones often reinforce this by brushing off their symptoms because they don’t understand them or know what to do. My goal is to educate you about what’s going on with your body to remove the fear that so often accompanies mysterious symptoms. This will help you feel more empowered to address your health.
Underlying mechanisms that cause symptoms and tissue damage with Covid-19
- High blood pressure
- Elevated heart rate
- Inflammation
- Tissue damage: The ACE-2 Receptor
Underlying mechanisms that cause symptoms and tissue damage with Covid-19
- High blood pressure
- Elevated heart rate
- Inflammation
- Tissue damage: The ACE-2 Receptor
The ACE-2 Receptor
ACE-2 receptors are on the surfaces of cells of tissues throughout our body, and their job is to modulate—or regulate—angiotensin-2. If ACE-2 is not able to do this, we see a rise in blood pressure, inflammation, and tissue damage throughout the whole body, along with potential damage to the lining of the blood vessels.
The problem with Covid-19 is that the virus binds to ACE-2 in order to enter the cell. As a result, ACE-2 can’t regulate angiotensin-2 effectively and the above problems are more likely to occur.
ACE-2 and endothelial cells
Endothelial cells make up the inner lining of our blood vessels. Researchers are finding Covid-19 patients have high amounts of inflammatory immune cells called macrophages and neutrophils in the endothelial lining, which indicates damage to this tissue. This is happening in endothelial tissue through the body, such as the lungs, kidney, heart, small intestines, pancreas, brain, and so forth. [2]
This explains why the patients who already had inflammatory diseases suffer the most severe symptoms. Imagine if you already have diabetes — the endothelial inflammation from Covid-19 puts your pancreas under even more duress, making it harder to regulate your blood sugar. Or if you already had high blood pressure, the inability to regulate angiotensin-2 suddenly makes your high blood pressure much riskier.
The damage to these tissues are what create the long-term effects in people who survive Covid-19 but experience lingering symptoms and worsening of their pre-existing health disorders.
The ACE-2 Receptor
ACE-2 receptors are on the surfaces of cells of tissues throughout our body, and their job is to modulate—or regulate—angiotensin-2. If ACE-2 is not able to do this, we see a rise in blood pressure, inflammation, and tissue damage throughout the whole body, along with potential damage to the lining of the blood vessels.
The problem with Covid-19 is that the virus binds to ACE-2 in order to enter the cell. As a result, ACE-2 can’t regulate angiotensin-2 effectively and the above problems are more likely to occur.
ACE-2 and endothelial cells
Endothelial cells make up the inner lining of our blood vessels. Researchers are finding Covid-19 patients have high amounts of inflammatory immune cells called macrophages and neutrophils in the endothelial lining, which indicates damage to this tissue. This is happening in endothelial tissue through the body, such as the lungs, kidney, heart, small intestines, pancreas, brain, and so forth. [2]
This explains why the patients who already had inflammatory diseases suffer the most severe symptoms. Imagine if you already have diabetes — the endothelial inflammation from Covid-19 puts your pancreas under even more duress, making it harder to regulate your blood sugar. Or if you already had high blood pressure, the inability to regulate angiotensin-2 suddenly makes your high blood pressure much riskier.
The damage to these tissues are what create the long-term effects in people who survive Covid-19 but experience lingering symptoms and worsening of their pre-existing health disorders.
Elevated Cytokines and Cytokine Storms
Cytokines are messenger proteins produced by immune cells that raise inflammation and promote excess coagulation of the blood. You can measure whether inflammation is a problem on a blood test by checking for D-dimer and fibrinogen. If these blood markers are elevated, this suggests hyper coagulation and cardiovascular tissue damage.
In many people, Covid-19 produces a cytokine storm, [3] or an over abundance of these inflammatory messenger cells, specifically interleukin-6 (IL-6). Inflammatory cytokines like IL-6 are necessary to fight infections, however Covid-19 patients produce an exaggerated inflammatory response and an overabundance of cytokines.
We see this on blood tests of Covid-19 patients who were sick one to two months ago. They are still very inflamed. This makes it harder for the blood to circulate, which can inflame the brain and cause symptoms of brain fog, fatigue, and malaise. It also exacerbates whatever pre-existing disorders you already had.[4] It basically makes it harder for all your body’s systems and organs to function.
Eight markers to run on a blood test to check for inflammation
You can test whether you have high inflammation by running the following blood markers:
Elevated Cytokines and Cytokine Storms
Cytokines are messenger proteins produced by immune cells that raise inflammation and promote excess coagulation of the blood. You can measure whether inflammation is a problem on a blood test by checking for D-dimer and fibrinogen. If these blood markers are elevated, this suggests hyper coagulation and cardiovascular tissue damage.
In many people, Covid-19 produces a cytokine storm, [3] or an over abundance of these inflammatory messenger cells, specifically interleukin-6 (IL-6). Inflammatory cytokines like IL-6 are necessary to fight infections, however Covid-19 patients produce an exaggerated inflammatory response and an overabundance of cytokines.
We see this on blood tests of Covid-19 patients who were sick one to two months ago. They are still very inflamed. This makes it harder for the blood to circulate, which can inflame the brain and cause symptoms of brain fog, fatigue, and malaise. It also exacerbates whatever pre-existing disorders you already had.[4] It basically makes it harder for all your body’s systems and organs to function.
Eight markers to run on a blood test to check for inflammation
You can test whether you have high inflammation by running the following blood markers:
C-reative protein (CRP)
High-density lipoprotein (HDL)
Interleukin-6 (IL-6)
Homocysteine
Sed Rate
Or erythrocyte sedimentation rate (ESR)
High-density lipoprotein (HDL)
Although this is normally seen as a marker for “good” cholesterol, if it’s over 85 this suggests inflammation
Ferritin
Uric Acid
Lactate dehydrogenase (LDH)
The reason I’m giving you this list is so you can check them all. If you only check one or two they may come back normal whereas the ones you didn’t check may be elevated.
When Covid-19 triggers an autoimmune response in the body
One of the most concerning things we’ve seen in our patients for whom we already had lab work is that Covid-19 triggers an autoimmune response in some people. [5][6] Autoimmunity is a permanent condition in which the immune system attacks and destroys tissue in the body.
This happens in part due to the inflammation, but also because Covid-19 cross reacts with different tissues in the body.[7] This means the virus has amino acid sequences that are identical to those in some body tissues (amino acids are the building blocks of proteins). When the immune system attacks the virus, it also can begin mistakenly attacking the identical amino acid sequences in body tissue, creating an autoimmune reaction that persists after the individual has recovered from Covid-19. Pre-existing inflammatory disorders raise the risk of this happening.
By the way, this mechanism is not unique to Covid-19 as a number of different viral and bacterial infections have been shown to trigger autoimmune reactions as well.[8][9] However, it seems to be more aggressive with Covid-19. The tissues that come under attack include the thyroid, pancreas, joints, the brain, the intestinal tract, and cellular mitochondria (the energy factory inside each cell).
The tissues that come under attack include:
THYROID
PANCREAS
JOINTS
BRAIN
INTESTINAL TRACT

MITOCHONDRIA
Some people also notice they develop food or chemical sensitivities after a Covid-19 infection. Again, this is likely the excess inflammation leading the immune system to become overly zealous and reactive to foods or chemicals in your environment. To dampen inflammation, strictly eliminate those foods from your diet and avoid irritating chemicals to the best of your ability, and follow an anti-inflammatory diet.
What to do if your inflammatory markers come back high
[11]Here’s the good news: If you see markers for elevated inflammation on a blood test, you can use simple diet, lifestyle, and nutrition strategies to calm down the inflammation.[10] Also, if you develop an autoimmune reaction post Covid-19, you will follow these same guidelines.
Although these are scientifically sound and effective strategies, they take work on your part. It means giving up some familiar foods and habits that are triggering your inflammation. But I can tell you after years in practice running one of the largest autoimmune clinics in the world, when patients discover how good they can feel and function, they come to love their new diet and habits.
Basic Strategies We Use With our Covid-19 Patients to Reduce Inflammation & Symptoms
These same strategies will also lower your risk of developing severe symptoms or reactions from Covid-19.[11]
C-reative protein (CRPn
High-density lipoprotein (HDL)
Interleukin-6 (IL-6)
Homocysteine
Sed Rate
Or erythrocyte sedimentation rate (ESR)
High-density lipoprotein (HDL)
Although this is normally seen as a marker for “good” cholesterol, if it’s over 85 this suggests inflammation
Ferritin
Uric Acid
Lactate dehydrogenase (LDH)
The reason I’m giving you this list is so you can check them all. If you only check one or two they may come back normal whereas the ones you didn’t check may be elevated.
When Covid-19 triggers an autoimmune response in the body
One of the most concerning things we’ve seen in our patients for whom we already had lab work is that Covid-19 triggers an autoimmune response in some people. [5][6] Autoimmunity is a permanent condition in which the immune system attacks and destroys tissue in the body.
This happens in part due to the inflammation, but also because Covid-19 cross reacts with different tissues in the body.[7] This means the virus has amino acid sequences that are identical to those in some body tissues (amino acids are the building blocks of proteins). When the immune system attacks the virus, it also can begin mistakenly attacking the identical amino acid sequences in body tissue, creating an autoimmune reaction that persists after the individual has recovered from Covid-19. Pre-existing inflammatory disorders raise the risk of this happening.
By the way, this mechanism is not unique to Covid-19 as a number of different viral and bacterial infections have been shown to trigger autoimmune reactions as well.[8][9] However, it seems to be more aggressive with Covid-19. The tissues that come under attack include the thyroid, pancreas, joints, the brain, the intestinal tract, and cellular mitochondria (the energy factory inside each cell).
The tissues that come under attack include:
One of the most concerning things we’ve seen in our patients for whom we already had lab work is that Covid-19 triggers an autoimmune response in some people. [5][6] Autoimmunity is a permanent condition in which the immune system attacks and destroys tissue in the body.
This happens in part due to the inflammation, but also because Covid-19 cross reacts with different tissues in the body.[7] This means the virus has amino acid sequences that are identical to those in some body tissues (amino acids are the building blocks of proteins). When the immune system attacks the virus, it also can begin mistakenly attacking the identical amino acid sequences in body tissue, creating an autoimmune reaction that persists after the individual has recovered from Covid-19. Pre-existing inflammatory disorders raise the risk of this happening.
By the way, this mechanism is not unique to Covid-19 as a number of different viral and bacterial infections have been shown to trigger autoimmune reactions as well.[8][9] However, it seems to be more aggressive with Covid-19. The tissues that come under attack include the thyroid, pancreas, joints, the brain, the intestinal tract, and cellular mitochondria (the energy factory inside each cell).
The tissues that come under attack include:
THYROID
PANCREAS
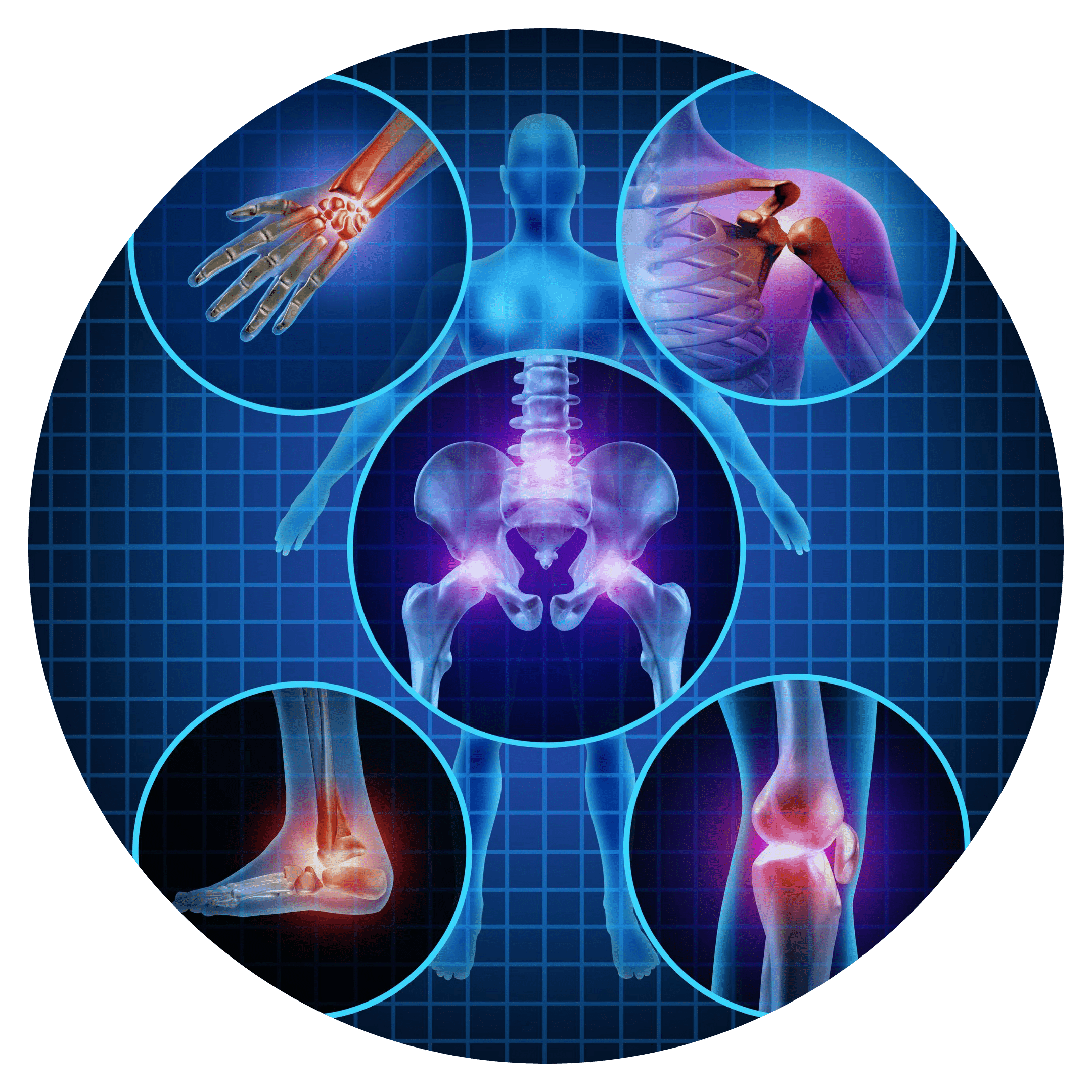
JOINTS
BRAIN
INTESTINAL TRACT

MITOCHONDRIA
Some people also notice they develop food or chemical sensitivities after a Covid-19 infection. Again, this is likely the excess inflammation leading the immune system to become overly zealous and reactive to foods or chemicals in your environment. To dampen inflammation, strictly eliminate those foods from your diet and avoid irritating chemicals to the best of your ability, and follow an anti-inflammatory diet.
Some people also notice they develop food or chemical sensitivities after a Covid-19 infection. Again, this is likely the excess inflammation leading the immune system to become overly zealous and reactive to foods or chemicals in your environment. To dampen inflammation, strictly eliminate those foods from your diet and avoid irritating chemicals to the best of your ability, and follow an anti-inflammatory diet.
What to do if your inflammatory markers come back high
[11]Here’s the good news: If you see markers for elevated inflammation on a blood test, you can use simple diet, lifestyle, and nutrition strategies to calm down the inflammation.[10] Also, if you develop an autoimmune reaction post Covid-19, you will follow these same guidelines.
Although these are scientifically sound and effective strategies, they take work on your part. It means giving up some familiar foods and habits that are triggering your inflammation. But I can tell you after years in practice running one of the largest autoimmune clinics in the world, when patients discover how good they can feel and function, they come to love their new diet and habits.
Basic Strategies We Use With our Covid-19 Patients to Reduce Inflammation & Symptoms
These same strategies will also lower your risk of developing severe symptoms or reactions from Covid-19.[11]
[11]Here’s the good news: If you see markers for elevated inflammation on a blood test, you can use simple diet, lifestyle, and nutrition strategies to calm down the inflammation.[10] Also, if you develop an autoimmune reaction post Covid-19, you will follow these same guidelines.
Although these are scientifically sound and effective strategies, they take work on your part. It means giving up some familiar foods and habits that are triggering your inflammation. But I can tell you after years in practice running one of the largest autoimmune clinics in the world, when patients discover how good they can feel and function, they come to love their new diet and habits.
Basic Strategies We Use With our Covid-19 Patients to Reduce Inflammation & Symptoms
These same strategies will also lower your risk of developing severe symptoms or reactions from Covid-19.[11]
30-Day Anti-Inflammatory Diet
Our first and most powerful strategy is to put our patients on an anti-inflammatory diet.[12][13] During the years of running our clinics, we have been testing patients—who come from all over the country and around the world— for food intolerances.[14][15][16] Removing these foods from their diet helps significantly in lowering inflammation.
Here are the food intolerances we see most often:
- Gluten: Gluten is by far the most inflammatory food we see in immune testing.
- Dairy: Dairy comes up about as often as gluten as being inflammatory.
- Soy
- Rice
- Corn
- Aspartame (artificial sweetener used in most diet beverages)
- Pork (and beef to a lesser degree)
- Eggs
If you follow an anti-inflammatory diet for 30 days that eliminates these foods along with sugars and other sweeteners, includes ample amounts of vegetables,[17][18] and removes processed and fast foods, this will profoundly reduce your inflammation. Additionally, I have my patients remove all grains, all legumes, and all nightshade vegetables (peppers, eggplants, tomatoes, and potatoes), and alcohol[19][20]. You can learn more by clicking on this link.
What can you eat? The foods you can eat on this diet include:
- Poultry
- Fish
- Lamb
- Vegetables (that aren’t nightshades)
- Fruits: Keep fruit consumption to a minimum because it is high in sugar, and eat fruit with fiber, protein, or fat to slow down the absorption of sugar.
- Healthy fats like olive oil, avocado oil, and coconut oil
How sugars and sweeteners promote no
Sugars and sweeteners (honey, maple syrup, agave, coconut sugar, etc.) are not included on an anti-inflammatory diet. This is because they cause a spike in your blood sugar, which is followed by a surge of insulin. This process is very pro-inflammatory every time it happens.[21][22][23] To lower inflammation, you absolutely need to avoid all sweeteners, sweet fruits (opt for lower glycemic fruit like raspberries), excess fruit, fruit juices, and fruit smoothies. If you eat a little fruit, slow down the sugar shock to your system by eating some fiber, protein, or fat with it.
Also, since most people have some sort of blood sugar imbalance, and because this diet is pretty limited, we want you to eat every two to three hours to keep your blood sugar stable. This doesn’t mean a full meal every two to three hours—eat your three main meals and include snacks in between. Your meals will be primarily meat and vegetables, and you can snack on nuts, seeds, meats, vegetables, and healthy fats. If you go too long without eating and get too hungry, you may not only cause your blood sugar to crash, but your hunger will make it a lot harder to stick to the diet.
Eat plenty of healthy fats with your meals and snacks not only to stay satiated, but also because fat is critical to good brain health. Your brain is made up of primarily fat, so the fats we eat have a large influence on our brain health.
Just one bite, or one small helping of something not allowed on the diet can undo all your good work.[24] Even just a crumb of gluten or dairy can trigger inflammation and make it harder for your system to calm down and find balance, so this is one diet where it’s important to be strict. Damaging inflammation can happen in as little as three minutes after eating something inflammatory and take three to six months to repair.
The good news is you can eat as much food as you’d like to stay satisfied and keep your energy levels up. This is not a diet to calorie count or minimize portions – most people lose weight on this diet. (Of course, don’t gorge yourself and eat excessively either, that also causes insulin surges and inflammation.)
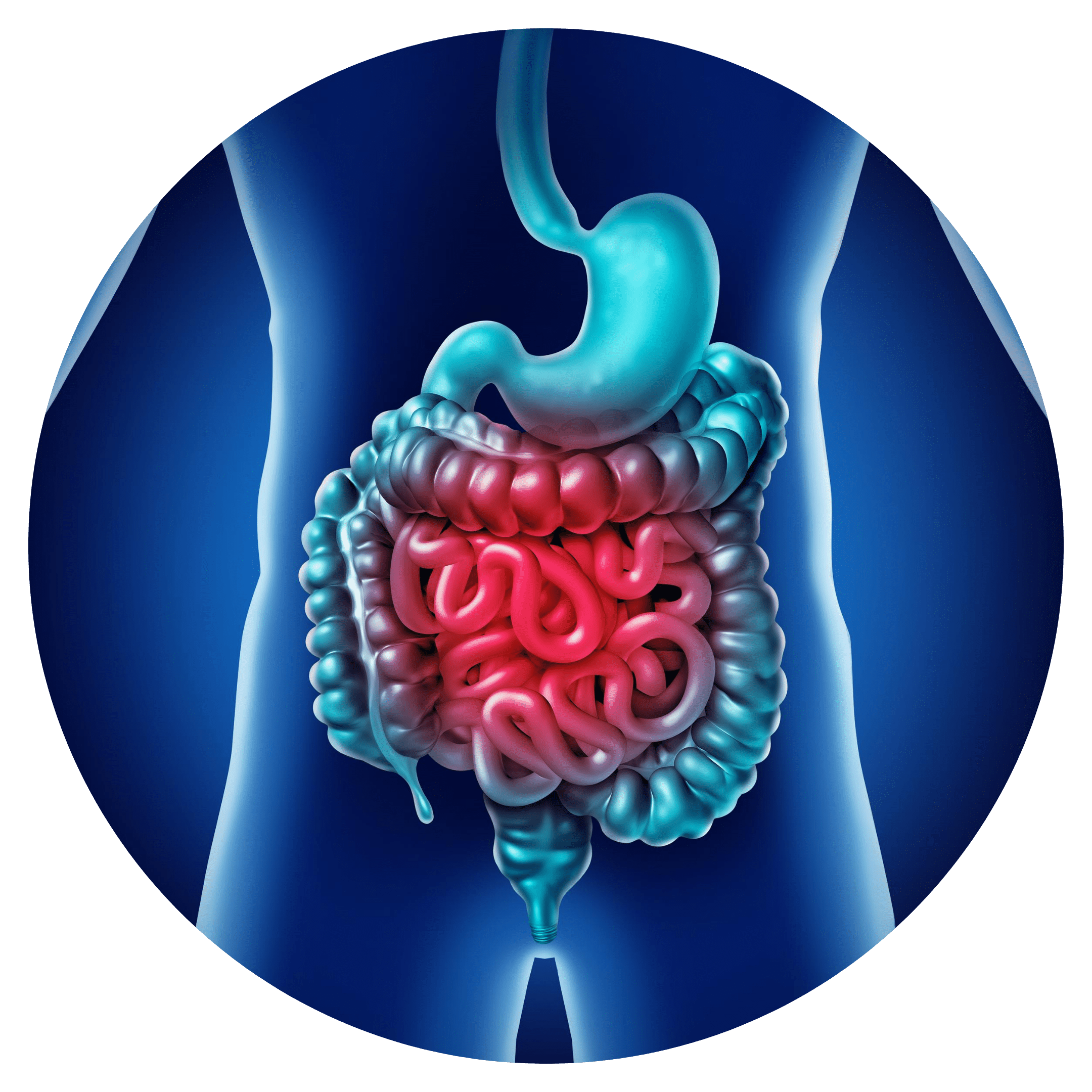
How intestinal permeability—or leaky gut—plays a role in inflammation and what to do about
Most people with chronic inflammation also have intestinal permeability. We also call this leaky gut. Over time, inflammation degrades the lining of the small intestine to the point where undigested food particles, bacteria, and other pathogens can escape from the digestive tract into the sterile environment of the bloodstream. This puts the immune system on red alert and causes inflammation throughout the body. Old injuries flare up and hurt, and the way inflammation manifests depends on your genetics. It can manifest as joint pain, skin disorders, respiratory problems, gut problems, or brain-based and mood issues. The worst part is it makes your existing inflammation even worse in a vicious feedback loop.
If you have leaky gut, you also most likely have leaky brain, or a permeable blood-brain barrier. This means the thin lining of cells that cover and protect the brain develops gaps or holes that allow particles into the brain that aren’t meant to be there, such as immune antibodies, bacteria, yeast, chemicals, heavy metals, and other pathogens. This inflames the brain and causes it to degenerate more quickly. Symptoms of leaky brain include brain fog (especially if it comes on after you eat), as well as fatigue, memory loss, depression, and anxiety.
As I mentioned earlier, leaky gut and leaky brain can happen in as little as three minutes after eating something inflammatory and take three to six months to repair. This is why so many people live in a constant state of inflammation—their immune barriers never get a chance to heal. The lungs, sinuses, and urogenital tract are other immune barriers that can be affected by inflammation.
After you have been on the autoimmune diet for 30 days, you start reintroducing foods one at a time every three days and monitor reactions. If you followed the diet carefully, your immune system will now be healthier and more robust, which can cause strong reactions to foods you weren’t aware were inflammatory for you. Reactions vary depending on the person, but look for symptoms in your gut, brain, skin, joints, or respiratory tract.
If you react to one of the foods you ate, go back on the anti-inflammatory diet until your inflammation calms down and permanently remove that food from your diet. Then move on to reintroducing a different food, repeating the process. Do this until you move through the list of foods you eliminated to determine which ones you react to.
Supplements to dampen inflammation
In addition to following the anti-inflammatory diet, certain supplements have been shown to be very effective in helping lower inflammation. These are the ones I use regularly in my practice:
Vitamin D
This one is foundational. Vitamin D increases immune cells called regulatory T-cells (T reg cells). As the name implies, T reg cells regulate whether you have a pro-inflammatory response or an anti-inflammatory response. When you support T reg cells with vitamin D they work to dampen inflammation. Vitamin D also supports the integrity of your immune barriers, such as the gut barrier, blood-brain barrier, and lung barrier so you’re better protected from inflammatory pathogens.
Therapeutic doses of vitamin D range from 10,000 to 20,000 IU a day, but make sure you and your doctor monitor your vitamin D levels regularly to make sure it doesn’t go too high. It’s rare to see levels go too high, but it’s best to stay aware of your vitamin D status.
Glutathione
This is probably the most powerful anti-inflammatory supplement out there. Glutathione is the body’s master antioxidant and necessary to protect cells and prevent inflammation.[26][27] But most people’s glutathione levels have been depleted by poor diets, excess sugars, environmental toxins, and chronic health conditions. Aging also depletes glutathione. Glutathione is especially important when the brain is inflamed as the brain’s immune system does not have an “off switch” like the body’s, so you need to intervene to dampen neuroinflammation to protect the brain tissue.
Glutathione also supports liver detoxification, decreases levels of pro-inflammatory immune cells, and supports the integrity of the gut, brain, and lung barriers. The two glutathione products we get the best results with are Trizomal Glutathione from Apex Energetics and Tri-Fortify Orange by Researched Nutritionals. You can also undergo glutathione IV therapy. How much you need depends on the degree of your inflammation, but we have our patients take 5–10 ml three times a day of Trizomal Glutathione.
Resveratrol
Taking therapeutic doses of resveratrol has been shown to significantly dampen inflammation, support healthy gut bacteria (the gut microbiome), and support the immune barriers. We find resveratrol has a profound impact on inflammation.[28]
You can use resveratrol capsules, but we like to use Resvero Active by Apex Energetics, which is a highly absorbable liposomal resveratrol and allows you to take therapeutic doses. How much resveratrol you take depends on how bad inflammation is, so take enough to feel an effect. We recommend 5–10 ml three times a day of Resvero Active.
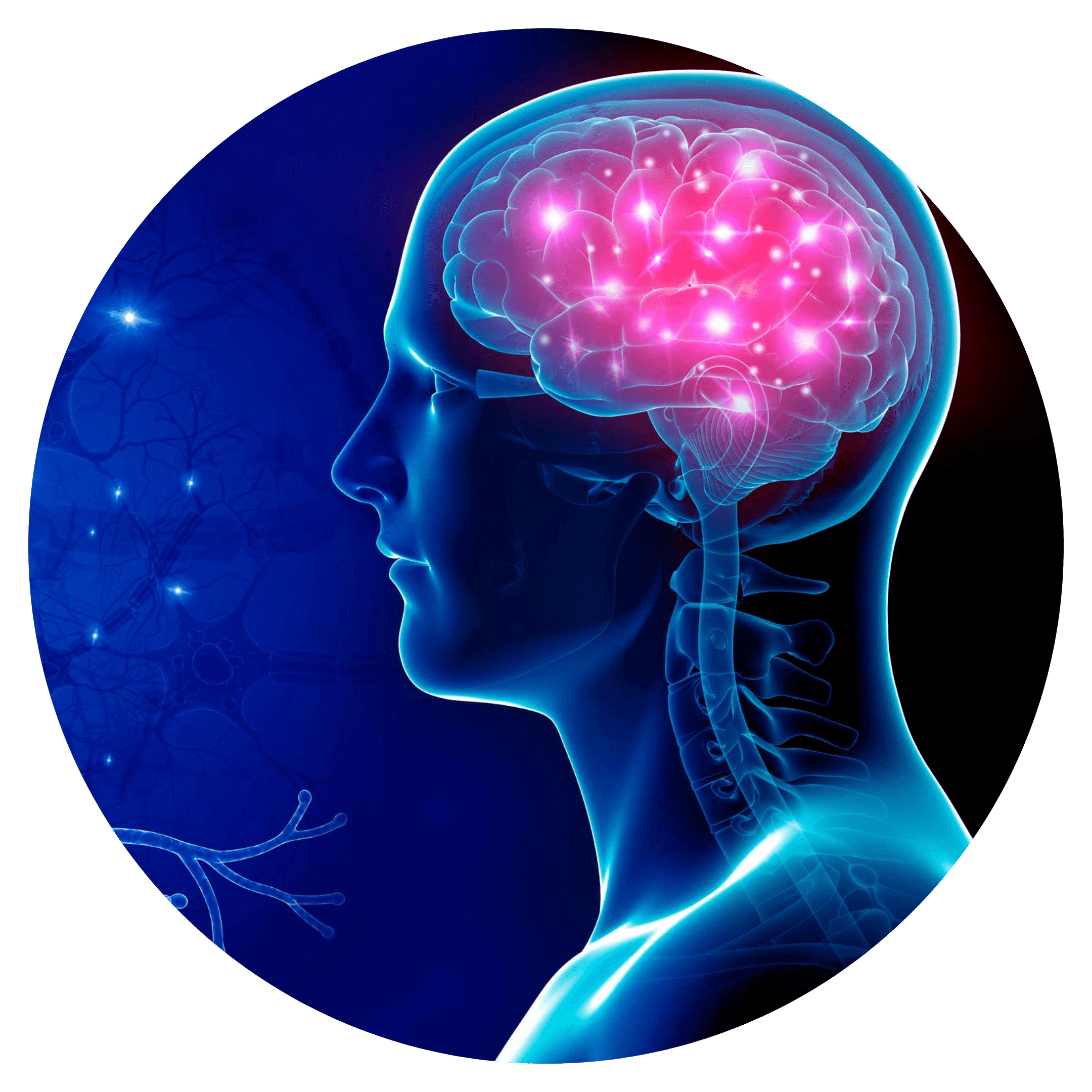
Why it’s important to address brain inflammation to dampen overall inflammation
One of the consequences of increased inflammation and cytokine storms is the brain becomes inflamed. Brain inflammation impairs brain function and speeds up the degeneration of brain tissue. Common symptoms of brain inflammation include brain fog, fatigue, memory loss, poor cognition, depression, loss of motivation, anxiety, irritability, and other brain-based and mood symptoms. Diminished brain function also leads to diminished organ function.
The brain communicates with the gut and the other organs via a large nerve called the vagus nerve.[29][30] However, in Covid-19 patients suffering from brain inflammation, we see poor communication between the brain and the gut, lungs, and heart and poorer function of those organs and systems as a result. Unfortunately, this triggers more inflammation in a vicious feedback loop. For instance, it can cause poor digestion, which in turn raises the risk of food intolerances and leaky gut.
Fortunately, we can exercise the vagus nerve to improve the brain’s communication with the organs and also to improve overall brain health.
These are the vagus nerve exercises I give my patients:

Gargle water as intensely as possible for three minutes, three times a day. Gargle to the point where you produce tears, or at least come close. The vagus originates in an area of the brain next to the area that produces tears, so if you can make yourself tear up then you know you’re doing a good job stimulating the vagus. It may take some time to work up to that.

Stimulate the gag reflex 10 times, three times a day using a tongue blade that you can buy off Amazon. Again, you want to do it to the point that you make your eyes tear.

Deep breathing exercises will help stimulate the vagus nerve as well as improve lung capacity and help oxygenate the body. Three times a day for five minutes at a time, breathe as deeply as you can through your nose and then exhale out your mouth. The goal is to minimize how many breaths you take per minute. Count your breaths and see if you can work towards cutting them in half. This builds lung capacity. I have people monitor their heart rate, blood pressure, and oxygen saturation while doing this exercise to ensure oxygen levels are actually going up.

Cold showers don’t sound great but they are important to incorporate into your routine. You can start with a warm shower and end with a warm shower, but at some point, bring the water to 60 degrees or lower for 60 seconds. Turn it as cold as it will go in the summer, and a little less than that in the winter and fall. If you can do it in the morning, it’s even better as it will boost your cortisol awakening response. Supporting your cortisol awakening response within 15 minutes of waking up has been shown to profoundly influence overall metabolic function and health. You may feel panicky and hyper ventilate the first few times, but when you get used to it, do deep breathing exercises while you’re in the cold shower. Soon you will come to love how the cold showers make you feel.
These exercises will help not only the vagus nerve but also brain plasticity, or the brain’s ability to develop new neural pathways. We only have a certain amount of neurons in our life spans—they are not cells we regenerate. We also lose neurons as we age, and dead neurons can impede communication among the neurons that are still viable. Therefore, the best way to maintain brain function and health as we age is by building more communication between the neurons we have left. We do this by constantly learning new things and developing positive habits.
However, for plasticity to work, you have to be consistent in performing these exercises and new habits for the new neuronal pathways to grow.
30-Day Anti-Inflammatory Diet
Our first and most powerful strategy is to put our patients on an anti-inflammatory diet.[12][13] During the years of running our clinics, we have been testing patients—who come from all over the country and around the world— for food intolerances.[14][15][16] Removing these foods from their diet helps significantly in lowering inflammation.
Here are the food intolerances we see most often:
- Gluten: Gluten is by far the most inflammatory food we see in immune testing.
- Dairy: Dairy comes up about as often as gluten as being inflammatory.
- Soy
- Rice
- Corn
- Aspartame (artificial sweetener used in most diet beverages)
- Pork (and beef to a lesser degree)
- Eggs
If you follow an anti-inflammatory diet for 30 days that eliminates these foods along with sugars and other sweeteners, includes ample amounts of vegetables,[17][18] and removes processed and fast foods, this will profoundly reduce your inflammation. Additionally, I have my patients remove all grains, all legumes, and all nightshade vegetables (peppers, eggplants, tomatoes, and potatoes), and alcohol[19][20]. You can learn more by clicking on this link.
What can you eat? The foods you can eat on this diet include:
- Poultry
- Fish
- Lamb
- Vegetables (that aren’t nightshades)
- Fruits: Keep fruit consumption to a minimum because it is high in sugar, and eat fruit with fiber, protein, or fat to slow down the absorption of sugar.
- Healthy fats like olive oil, avocado oil, and coconut oil
How sugars and sweeteners promote no
Sugars and sweeteners (honey, maple syrup, agave, coconut sugar, etc.) are not included on an anti-inflammatory diet. This is because they cause a spike in your blood sugar, which is followed by a surge of insulin. This process is very pro-inflammatory every time it happens.[21][22][23] To lower inflammation, you absolutely need to avoid all sweeteners, sweet fruits (opt for lower glycemic fruit like raspberries), excess fruit, fruit juices, and fruit smoothies. If you eat a little fruit, slow down the sugar shock to your system by eating some fiber, protein, or fat with it.
Also, since most people have some sort of blood sugar imbalance, and because this diet is pretty limited, we want you to eat every two to three hours to keep your blood sugar stable. This doesn’t mean a full meal every two to three hours—eat your three main meals and include snacks in between. Your meals will be primarily meat and vegetables, and you can snack on nuts, seeds, meats, vegetables, and healthy fats. If you go too long without eating and get too hungry, you may not only cause your blood sugar to crash, but your hunger will make it a lot harder to stick to the diet.
Eat plenty of healthy fats with your meals and snacks not only to stay satiated, but also because fat is critical to good brain health. Your brain is made up of primarily fat, so the fats we eat have a large influence on our brain health.
Just one bite, or one small helping of something not allowed on the diet can undo all your good work.[24] Even just a crumb of gluten or dairy can trigger inflammation and make it harder for your system to calm down and find balance, so this is one diet where it’s important to be strict. Damaging inflammation can happen in as little as three minutes after eating something inflammatory and take three to six months to repair.
The good news is you can eat as much food as you’d like to stay satisfied and keep your energy levels up. This is not a diet to calorie count or minimize portions – most people lose weight on this diet. (Of course, don’t gorge yourself and eat excessively either, that also causes insulin surges and inflammation.)
How intestinal permeability—or leaky gut—plays a role in inflammation and what to do about
Most people with chronic inflammation also have intestinal permeability. We also call this leaky gut. Over time, inflammation degrades the lining of the small intestine to the point where undigested food particles, bacteria, and other pathogens can escape from the digestive tract into the sterile environment of the bloodstream. This puts the immune system on red alert and causes inflammation throughout the body. Old injuries flare up and hurt, and the way inflammation manifests depends on your genetics. It can manifest as joint pain, skin disorders, respiratory problems, gut problems, or brain-based and mood issues. The worst part is it makes your existing inflammation even worse in a vicious feedback loop.
If you have leaky gut, you also most likely have leaky brain, or a permeable blood-brain barrier. This means the thin lining of cells that cover and protect the brain develops gaps or holes that allow particles into the brain that aren’t meant to be there, such as immune antibodies, bacteria, yeast, chemicals, heavy metals, and other pathogens. This inflames the brain and causes it to degenerate more quickly. Symptoms of leaky brain include brain fog (especially if it comes on after you eat), as well as fatigue, memory loss, depression, and anxiety.
As I mentioned earlier, leaky gut and leaky brain can happen in as little as three minutes after eating something inflammatory and take three to six months to repair. This is why so many people live in a constant state of inflammation—their immune barriers never get a chance to heal. The lungs, sinuses, and urogenital tract are other immune barriers that can be affected by inflammation.
After you have been on the autoimmune diet for 30 days, you start reintroducing foods one at a time every three days and monitor reactions. If you followed the diet carefully, your immune system will now be healthier and more robust, which can cause strong reactions to foods you weren’t aware were inflammatory for you. Reactions vary depending on the person, but look for symptoms in your gut, brain, skin, joints, or respiratory tract.
If you react to one of the foods you ate, go back on the anti-inflammatory diet until your inflammation calms down and permanently remove that food from your diet. Then move on to reintroducing a different food, repeating the process. Do this until you move through the list of foods you eliminated to determine which ones you react to.
Supplements to dampen inflammation
In addition to following the anti-inflammatory diet, certain supplements have been shown to be very effective in helping lower inflammation. These are the ones I use regularly in my practice:
Vitamin D
This one is foundational. Vitamin D increases immune cells called regulatory T-cells (T reg cells). As the name implies, T reg cells regulate whether you have a pro-inflammatory response or an anti-inflammatory response. When you support T reg cells with vitamin D they work to dampen inflammation. Vitamin D also supports the integrity of your immune barriers, such as the gut barrier, blood-brain barrier, and lung barrier so you’re better protected from inflammatory pathogens.
Therapeutic doses of vitamin D range from 10,000 to 20,000 IU a day, but make sure you and your doctor monitor your vitamin D levels regularly to make sure it doesn’t go too high. It’s rare to see levels go too high, but it’s best to stay aware of your vitamin D status.
Glutathione
This is probably the most powerful anti-inflammatory supplement out there. Glutathione is the body’s master antioxidant and necessary to protect cells and prevent inflammation.[26][27] But most people’s glutathione levels have been depleted by poor diets, excess sugars, environmental toxins, and chronic health conditions. Aging also depletes glutathione. Glutathione is especially important when the brain is inflamed as the brain’s immune system does not have an “off switch” like the body’s, so you need to intervene to dampen neuroinflammation to protect the brain tissue.
Glutathione also supports liver detoxification, decreases levels of pro-inflammatory immune cells, and supports the integrity of the gut, brain, and lung barriers. The two glutathione products we get the best results with are Trizomal Glutathione from Apex Energetics and Tri-Fortify Orange by Researched Nutritionals. You can also undergo glutathione IV therapy. How much you need depends on the degree of your inflammation, but we have our patients take 5–10 ml three times a day of Trizomal Glutathione.
Resveratrol
Taking therapeutic doses of resveratrol has been shown to significantly dampen inflammation, support healthy gut bacteria (the gut microbiome), and support the immune barriers. We find resveratrol has a profound impact on inflammation.[28]
You can use resveratrol capsules, but we like to use Resvero Active by Apex Energetics, which is a highly absorbable liposomal resveratrol and allows you to take therapeutic doses. How much resveratrol you take depends on how bad inflammation is, so take enough to feel an effect. We recommend 5–10 ml three times a day of Resvero Active.
Why it’s important to address brain inflammation to dampen overall inflammation
One of the consequences of increased inflammation and cytokine storms is the brain becomes inflamed. Brain inflammation impairs brain function and speeds up the degeneration of brain tissue. Common symptoms of brain inflammation include brain fog, fatigue, memory loss, poor cognition, depression, loss of motivation, anxiety, irritability, and other brain-based and mood symptoms. Diminished brain function also leads to diminished organ function.
The brain communicates with the gut and the other organs via a large nerve called the vagus nerve.[29][30] However, in Covid-19 patients suffering from brain inflammation, we see poor communication between the brain and the gut, lungs, and heart and poorer function of those organs and systems as a result. Unfortunately, this triggers more inflammation in a vicious feedback loop. For instance, it can cause poor digestion, which in turn raises the risk of food intolerances and leaky gut.
Fortunately, we can exercise the vagus nerve to improve the brain’s communication with the organs and also to improve overall brain health.
These are the vagus nerve exercises I give my patients:

Gargle water as intensely as possible for three minutes, three times a day. Gargle to the point where you produce tears, or at least come close. The vagus originates in an area of the brain next to the area that produces tears, so if you can make yourself tear up then you know you’re doing a good job stimulating the vagus. It may take some time to work up to that.

Stimulate the gag reflex 10 times, three times a day using a tongue blade that you can buy off Amazon. Again, you want to do it to the point that you make your eyes tear.

Deep breathing exercises will help stimulate the vagus nerve as well as improve lung capacity and help oxygenate the body. Three times a day for five minutes at a time, breathe as deeply as you can through your nose and then exhale out your mouth. The goal is to minimize how many breaths you take per minute. Count your breaths and see if you can work towards cutting them in half. This builds lung capacity. I have people monitor their heart rate, blood pressure, and oxygen saturation while doing this exercise to ensure oxygen levels are actually going up.

Cold showers don’t sound great but they are important to incorporate into your routine. You can start with a warm shower and end with a warm shower, but at some point, bring the water to 60 degrees or lower for 60 seconds. Turn it as cold as it will go in the summer, and a little less than that in the winter and fall. If you can do it in the morning, it’s even better as it will boost your cortisol awakening response. Supporting your cortisol awakening response within 15 minutes of waking up has been shown to profoundly influence overall metabolic function and health. You may feel panicky and hyper ventilate the first few times, but when you get used to it, do deep breathing exercises while you’re in the cold shower. Soon you will come to love how the cold showers make you feel.
These exercises will help not only the vagus nerve but also brain plasticity, or the brain’s ability to develop new neural pathways. We only have a certain amount of neurons in our life spans—they are not cells we regenerate. We also lose neurons as we age, and dead neurons can impede communication among the neurons that are still viable. Therefore, the best way to maintain brain function and health as we age is by building more communication between the neurons we have left. We do this by constantly learning new things and developing positive habits.
However, for plasticity to work, you have to be consistent in performing these exercises and new habits for the new neuronal pathways to grow.

Dr. Josh Redd
DC, MS, DABFM, DAAIM
Industry Leader in Functional & Personalized Medicine
Josh Redd, DC, MS, DABFM, DAAIM, is the founder of RedRiver Health and Wellness, bestselling author of The Truth About Low Thyroid, co-host of ABC’s The Younger You, which received an Emmy Nomination.
RedRiver Health and Wellness currently consists of seven functional medicine clinics across the western United States focusing on challenging autoimmune, neurological and endocrine disorders.
With hundreds of patients from around the world in his clinics daily, Dr. Redd is able to quickly identify patterns and trends among his patient population, as well as which evidence-based clinical strategies are the most successful in managing autoimmunity.
A Chiropractic Physician, a Diplomate in Functional Medicine from the American Board of Functional Medicine and a Diplomate in Integrative Medicine from the American Association of Integrative Medicine, Dr. Redd was recently accepted into the #1 ranked public health program in the country at Johns Hopkins with an emphasis on molecular microbiology and immunology.
Dr. Redd trains closely with Dr. Datis Kharrazian, PhD, DHSc, DC, MS, MMSc, FACN, Harvard Medical School Research Fellow and Dr. Aristo Vojdani, PhD, MSc and credits them for much of his success throughout the last 10 years as a functional medicine practitioner.
Dr. Redd delivers post-graduate lectures to health care professionals around the country on functional medicine topics such as neuroendocrine immunology, gastrointestinal disorders, gluten sensitivity and celiac disease, autoimmune management, functional blood chemistry, and clinical strategies for hypothyroidism and Hashimoto’s.

Dr. Josh Redd
DC, MS, DABFM, DAAIM
Industry Leader in Functional & Personalized Medicine
Josh Redd, DC, MS, DABFM, DAAIM, is the founder of RedRiver Health and Wellness, bestselling author of The Truth About Low Thyroid, co-host of ABC’s The Younger You, which received an Emmy Nomination.
RedRiver Health and Wellness currently consists of seven functional medicine clinics across the western United States focusing on challenging autoimmune, neurological and endocrine disorders.
With hundreds of patients from around the world in his clinics daily, Dr. Redd is able to quickly identify patterns and trends among his patient population, as well as which evidence-based clinical strategies are the most successful in managing autoimmunity.
A Chiropractic Physician, a Diplomate in Functional Medicine from the American Board of Functional Medicine and a Diplomate in Integrative Medicine from the American Association of Integrative Medicine, Dr. Redd was recently accepted into the #1 ranked public health program in the country at Johns Hopkins with an emphasis on molecular microbiology and immunology.
Dr. Redd trains closely with Dr. Datis Kharrazian, PhD, DHSc, DC, MS, MMSc, FACN, Harvard Medical School Research Fellow and Dr. Aristo Vojdani, PhD, MSc and credits them for much of his success throughout the last 10 years as a functional medicine practitioner.
Dr. Redd delivers post-graduate lectures to health care professionals around the country on functional medicine topics such as neuroendocrine immunology, gastrointestinal disorders, gluten sensitivity and celiac disease, autoimmune management, functional blood chemistry, and clinical strategies for hypothyroidism and Hashimoto’s.
Covid-19 Long Haul References
Bourgonje AR, Abdulle AE, Timens W, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) [published online ahead of print, 2020 May 17]. J Pathol. 2020;10.1002/path.5471. doi:10.1002/path.5471
2 Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020;190:62. doi:10.1016/j.thromres.2020.04.014
3 Mahmudpour M, Roozbeh J, Keshavarz M, Farrokhi S, Nabipour I. COVID-19 cytokine storm: The anger of inflammation [published online ahead of print, 2020 May 30]. Cytokine. 2020;133:155151. doi:10.1016/j.cyto.2020.155151
4 Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020;8(6):e46-e47. doi:10.1016/S2213-2600(20)30216-2
5 Amiral J, Vissac AM, Seghatchian J. Covid-19, induced activation of hemostasis, and immune reactions: Can an auto-immune reaction contribute to the delayed severe complications observed in some patients?. Transfus Apher Sci. 2020;59(3):102804. doi:10.1016/j.transci.2020.102804
6 Zhou, Yaqing et al. “Clinical and Autoimmune Characteristics of Severe and Critical Cases of COVID-19.” Clinical and translational science, 10.1111/cts.12805. 21 Apr. 2020, doi:10.1111/cts.12805
7 Vojdani, Kharrazian. “Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases.” Letter to the editor. Clinical Immunology. Available online 24 May 2020, 108480. https://doi.org/10.1016/j.clim.2020.108480
8 Augustyniak D, Majkowska-Skrobek G, Roszkowiak J, Dorotkiewicz-Jach A. Defensive and Offensive Cross-Reactive Antibodies Elicited by Pathogens: The Good, the Bad and the Ugly. Curr Med Chem. 2017;24(36):4002-4037. doi:10.2174/0929867324666170508110222
9 Segal Y, Shoenfeld Y. Vaccine-induced autoimmunity: the role of molecular mimicry and immune crossreaction. Cell Mol Immunol. 2018;15(6):586-594. doi:10.1038/cmi.2017.151
10 Myles, Ian A. “Fast food fever: reviewing the impacts of the Western diet on immunity.” Nutrition journal vol. 13 61. 17 Jun. 2014, doi:10.1186/1475-2891-13-61
11 Schett, Georg et al. “COVID-19: risk for cytokine targeting in chronic inflammatory diseases?.” Nature reviews. Immunology vol. 20,5 (2020): 271-272. doi:10.1038/s41577-020-0312-7
12 Whalen, Kristine A et al. “Paleolithic and Mediterranean Diet Pattern Scores Are Inversely Associated with Biomarkers of Inflammation and Oxidative Balance in Adults.” The Journal of nutrition vol. 146,6 (2016): 1217-26. doi:10.3945/jn.115.224048
13 Abbott, Robert D et al. “Efficacy of the Autoimmune Protocol Diet as Part of a Multi-disciplinary, Supported Lifestyle Intervention for Hashimoto’s Thyroiditis.” Cureus vol. 11,4 e4556. 27 Apr. 2019, doi:10.7759/cureus.4556
14 Choudhary, Arbind Kumar, and Etheresia Pretorius. “Revisiting the safety of aspartame.” Nutrition reviews vol. 75,9 (2017): 718-730. doi:10.1093/nutrit/nux035
15 Liu, Chih-Wei et al. “Quantitative proteomics reveals systematic dysregulations of liver protein metabolism in sucralose-treated mice.” Journal of proteomics vol. 196 (2019): 1-10. doi:10.1016/j.jprot.2019.01.011
16 Bian, Xiaoming et al. “Gut Microbiome Response to Sucralose and Its Potential Role in Inducing Liver Inflammation in Mice.” Frontiers in physiology vol. 8 487. 24 Jul. 2017, doi:10.3389/fphys.2017.00487
17 Koh, Ara et al. “From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites.” Cell vol. 165,6 (2016): 1332-1345. doi:10.1016/j.cell.2016.05.041
18 Levy, Maayan et al. “Microbiome, metabolites and host immunity.” Current opinion in microbiology vol. 35 (2017): 8-15. doi:10.1016/j.mib.2016.10.003
19 Szabo, Gyongyi, and Banishree Saha. “Alcohol’s Effect on Host Defense.” Alcohol research : current reviews vol. 37,2 (2015): 159-70.
20 Engen, Phillip A et al. “The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota.” Alcohol research : current reviews vol. 37,2 (2015): 223-36.
21 Albert Sanchez, J. L. Reeser, H. S. Lau, P. Y. Yahiku, R. E. Willard, P. J. McMillan, S. Y. Cho, A. R. Magie, U. D. Register, Role of sugars in human neutrophilic phagocytosis, The American Journal of Clinical Nutrition, Volume 26, Issue 11, November 1973, Pages 1180–1184, https://doi.org/10.1093/ajcn/26.11.1180
22 Butler, Michael J, and Ruth M Barrientos. “The impact of nutrition on COVID-19 susceptibility and long-term consequences.” Brain, behavior, and immunity, S0889-1591(20)30537-7. 18 Apr. 2020, doi:10.1016/j.bbi.2020.04.040
23 Freeman, Clara R et al. “Impact of sugar on the body, brain, and behavior.” Frontiers in bioscience (Landmark edition) vol. 23 2255-2266. 1 Jun. 2018
24 Caio, G., Volta, U., Tovoli, F. et al. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol 14, 26 (2014). https://doi.org/10.1186/1471-230X-14-26
25 Grant, William B et al. “Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths.” Nutrients vol. 12,4 E988. 2 Apr. 2020, doi:10.3390/nu12040988
26 Checconi, Paola et al. “Role of Glutathionylation in Infection and Inflammation.” Nutrients vol. 11,8 1952. 20 Aug. 2019, doi:10.3390/nu11081952
27 Horowitz, Richard I et al. “Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: A report of 2 cases.” Respiratory medicine case reports, vol. 30 101063. 21 Apr. 2020, doi:10.1016/j.rmcr.2020.101063
28 Malaguarnera L. Influence of Resveratrol on the Immune Response. Nutrients. 2019;11(5):946. Published 2019 Apr 26. doi:10.3390/nu11050946
29 Yuan, Hsiangkuo, and Stephen D Silberstein. “Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part I.” Headache vol. 56,1 (2016): 71-8. doi:10.1111/head.12647
30 Bonaz, B et al. “Vagal tone: effects on sensitivity, motility, and inflammation.” Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society vol. 28,4 (2016): 455-62. doi:10.1111/nmo.12817
Disclaimer: Statements on this website have not been evaluated by the Food and Drug Administration. Products are not intended to diagnose, treat, cure or prevent any disease.
You should always consult with your healthcare practitioner prior to starting any new dietary supplement or program.
The information provided on this site is for informational purposes only and is not intended as a substitute for advice from your physician or other healthcare professional or any information contained on or in any product label or packaging. You should not use the information on this site for diagnosis or treatment of any health problem or for prescription of any medication or other treatment. Always consult with a healthcare professional before starting any diet, exercise or supplementation program, before taking any medication, or if you have or suspect you might have a health problem. You should not stop taking any medication without first consulting your physician.
As individuals differ, so will results. Always check with your doctor for risks associated with dietary supplements and your specific health conditions and/or allergies.